Credentialing is more than filling out forms. Each application has to match licensing data exactly. One incorrect date or missing document can result in months of delay for the credentialing candidate. Let us get you credentialed! Our comprehensive medical credentialing services simplify enrollment so you can join the top insurance payers’ networks effortlessly. Time to get your revenue rolling!

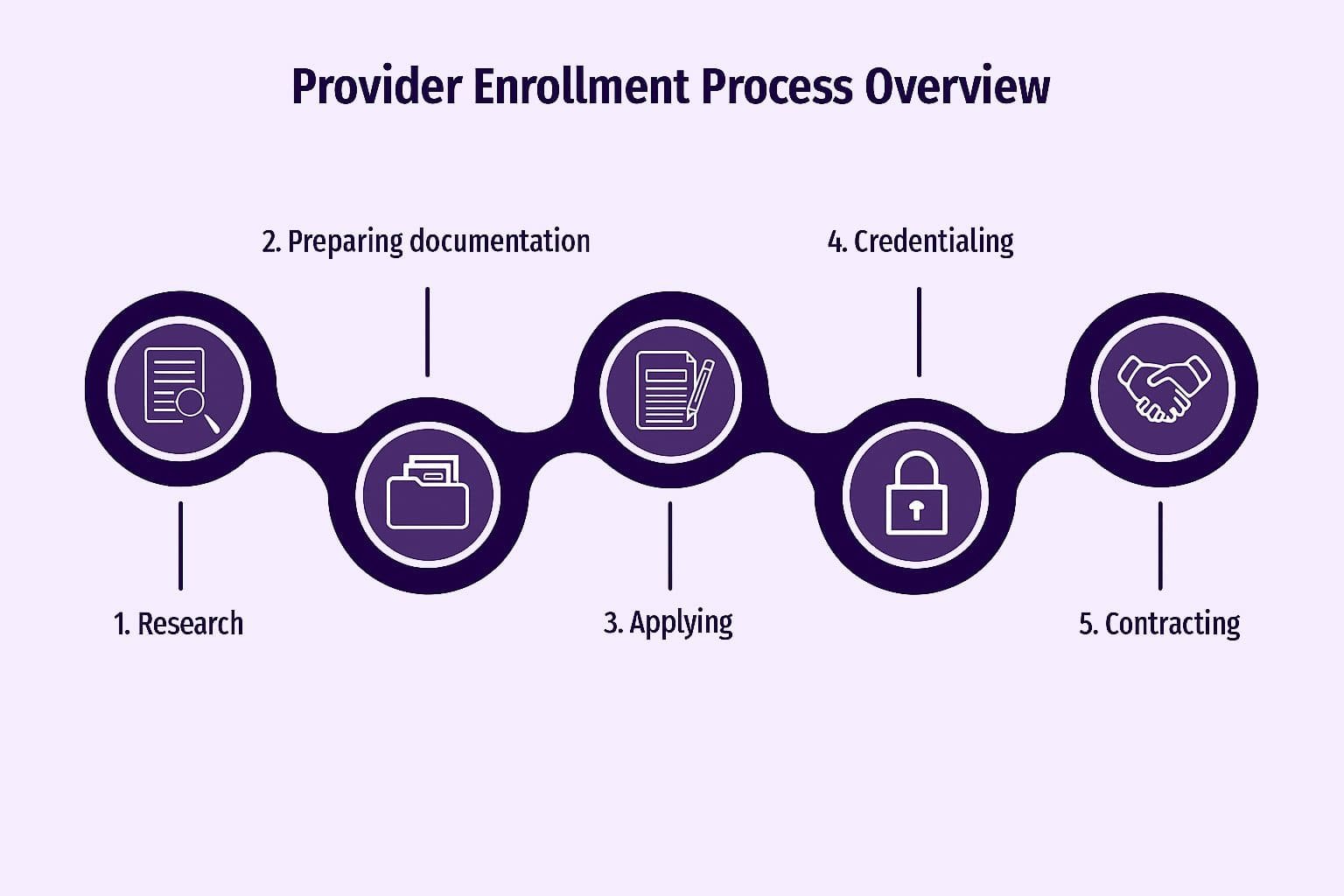
Embarking on the credentialing journey can feel like navigating a maze. Between CAQH, PECOS, payer panels, and hospital privileges, things get messy fast. But missing a step can mean lost revenue, delayed claims, and frustrated staff. Let’s look at how provider credentialing services and medical credentialing for physicians can streamline healthcare credentialing, reduce delays, and optimize your Healthcare Revenue Cycle Management (RCM).
We manage your documentation, registration, verification, and panel applications so you can join networks quickly and cleanly. Speed up claims with EDI, EFT, and ERA enrollment. No more manual mishaps or payment delays. Whether you’re an MD, NP, PA, dentist, pathologist, or radiologist, we make sure you’re connected with commercial and government payers. Need privileges? We handle committee forms, documentation, and follow-ups. With CAQH ProView and PECOS backing, your primary-source verified data stays up-to-date and accessible. We secure and renew licenses across states critical for telehealth or multi-state practice. Our negotiators help drive favorable terms on fees, splits, and contract language. We track expiry dates, re-attest CAQH, and renew payer and hospital approvals proactively.


Cost‑Effectiveness and Data Security
Outsourcing can cost $200–$400 per provider initially versus $85,000/year for a full-time specialist. Plus, we adhere to HIPAA and encryption standards.
Reduced Administrative Burden & Documentation Overload
Let your staff refocus on patient care—credentialing paperwork is our domain.
Streamlined Process Through Direct Payer Communication
Our experience means fewer back-and-forths and faster credential approvals with payers.
Accelerated Enrollment & Contract Execution: Becoming In‑Network Faster
Onboarding times drop 30–50%, so you can bill sooner.
Leveraging Specialized Expertise for Optimal Outcomes
Our team handles CAQH, PECOS, licensing, payer nuances—and they do it often.
Stop losing money to delays. Let our provider credentialing services and medical licensing services take it off your plate. Increase your net collection ratio, reduce denials, and onboard seamlessly as an in-network provider.
Schedule your consultation today and start your journey towards a healthier Revenue Cycle Management. Contact us now!
Typically 90–180 days, but outsourcing cuts that by 30–50%.
No, you get full visibility through our secure portal and live updates.
CAQH is used by commercial payers; PECOS is for Medicare enrollment.
Absolutely, our Healthcare Licensing Services cover interstate credentialing and IMLC.
Yes, timely credentialing ensures cleaner claims, fewer rejections, and faster payments.

Accurate billing, faster reimbursements, better cash flow. Your practice deserves the MediDoc Care MD advantage.
MediDoc Care MD © 2025 All Rights Reserved.